A Full Guide to Botox for Dentists
Dentists are increasingly using Botox to treat TMJ disorders, bruxism, and orofacial pain by relaxing overactive jaw muscles and easing strain on the temporomandibular joint. Botox blocks acetylcholine release to reduce muscle contractions and pain, offering a reliable alternative to treatments like night guards. It can also soften facial wrinkles as a secondary benefit. Common injection sites include the masseter, temporalis, and medial pterygoid muscles. Additional therapies like muscle stretching, trigger point treatments, and soft food diets can help enhance and maintain results.
Table of Contents
Cosmetic vs. Therapeutic Botox
Understanding TMD and Orofacial Pain
Will Therapeutic Botox Fix My Wrinkles?
Can Dentists Administer Botox?
How to Learn Botox for Dentists
What Techniques Are Used When Administering Botox for Therapeutics?
Botox vs. Night Guards To Treat TMJ Pain
Additional Remedies for Treating TMJ-Related Muscle Pain
For years, dentists have searched for more effective ways to relieve TMJ disorder and orofacial pain beyond traditional treatments. Botox, widely recognized for its cosmetic applications, is now proving to be a valuable tool in dentistry. Dentists can leverage Botox as an effective solution for treating TMJ disorder, orofacial pain, and other muscle-related dental issues. Traditional treatments such as night guards, warm and cold packs, and dietary modifications often require strict patient compliance, which can be inconsistent. Botox provides a more reliable alternative by directly targeting the muscles responsible for TMJ pain, offering relief regardless of patient adherence to at-home therapies.
By inhibiting acetylcholine release at the neuromuscular junction, Botox reduces muscle contractions, easing tension and alleviating discomfort. When applied correctly, it can significantly improve jaw function and provide long-term relief for patients struggling with chronic TMJ symptoms. As more dental professionals recognize its benefits, integrating Botox into practice has the potential to transform pain management in dentistry, offering a non-invasive, effective solution for conditions that have traditionally been difficult to treat. This guide will provide a comprehensive overview of Botox in dentistry, from its mechanism of action to practical applications, helping dentists confidently incorporate this treatment into their practice.
What Is Botox?
Botox is a neurotoxin derived from botulinum toxin that temporarily relaxes muscles by blocking nerve signals. While widely known for its cosmetic benefits, its use in dentistry is gaining traction for treating TMJ disorders, bruxism, and orofacial pain. Originally developed by Allergan, Botox has become a generic term for similar neurotoxins, including Dysport and Xeomin, which function in the same way. In dental procedures, Botox is injected into overactive jaw muscles to alleviate jaw stiffness, reduce excessive muscle contractions, and address common symptoms of TMJ disorders. By inhibiting involuntary muscle movements, it offers pain relief and improved function for patients experiencing persistent discomfort.
Cosmetic vs. Therapeutic Botox
Botox has long been associated with cosmetic enhancements, helping individuals achieve a more youthful appearance by smoothing out wrinkles caused by repetitive facial expressions like smiling and frowning. By temporarily relaxing targeted muscles, Botox reduces the visibility of dynamic wrinkles, making it a popular choice for those seeking aesthetic improvements. However, beyond its cosmetic appeal, Botox has emerged as a powerful therapeutic tool in dentistry. Excessive muscle contractions in the jaw can lead to conditions such as bruxism and TMJ disorders, causing persistent discomfort and pain. When administered by a qualified healthcare professional, Botox helps regulate pain signals and alleviates ongoing pain by relaxing overactive jaw muscles. This dual functionality makes Botox a versatile treatment option—whether for cosmetic refinement or to improve the quality of life for patients experiencing chronic muscle-related dental issues.
Understanding TMD and Orofacial Pain
Temporomandibular disorder (TMD) refers to the dysfunction of the temporomandibular joint due to chronic overuse, often leading to structural and muscular complications. While TMJ refers specifically to the joint itself, TMD encompasses the range of conditions that affect it, including pain, muscle hypertrophy, and restricted movement. Persistent bruxism and clenching place excessive stress on the joint, leading to deterioration of the protective disc between the jawbone and skull. This disc can become displaced or flattened, resulting in what is known as TMJ derangement. In severe cases, patients may experience a locked jaw—either in an open or closed position—due to the improper positioning of the disc. These complications can lead to chronic discomfort, difficulty in chewing, and recurring headaches. Without timely intervention, TMD can progress, affecting both oral health and overall quality of life.
The temporomandibular joint (TMJ), commonly referred to as the jaw joint, plays a crucial role in essential functions such as chewing, speaking, and facial movements. This joint, along with the muscles of mastication—including the masseter, temporalis, medial pterygoid, and lateral pterygoid—works continuously to facilitate jaw movement. However, excessive strain on these muscles, often caused by bruxism (teeth grinding and clenching), can lead to hyperactivity and chronic overuse, resulting in significant facial pain and discomfort. Many individuals suffer from these issues unknowingly, as bruxism frequently occurs involuntarily during sleep. As a result, patients may experience symptoms such as morning headaches, jaw stiffness, clicking or popping sounds when opening the mouth, and persistent discomfort in the jaw and surrounding muscles.
Left untreated, TMJ disorders can lead to severe dental complications, including excessive tooth wear, gum recession, and even structural damage to the temporomandibular joint itself. Many sufferers endure years of discomfort without seeking treatment, simply accepting their pain as a normal part of life. While neurologists may use Botox to manage migraine headaches, they often overlook the role of the masticatory muscles, leaving patients with unresolved muscle pain. Similar to how repetitive muscle contractions build strength in the body, chronic clenching and grinding can cause the jaw muscles to enlarge and become more painful over time. This can result in headaches radiating from behind the eyes, across the forehead, and into the base of the skull. Traditional treatment options such as night guards and orthotics provide some relief, but many patients go undiagnosed for years before seeking effective intervention. Understanding the connection between TMJ disorders and facial pain is key to early diagnosis and comprehensive treatment.
Botox Mechanism of Action
Botox functions by temporarily inhibiting the release of acetylcholine, a neurotransmitter responsible for muscle contractions, at the neuromuscular junction. This process prevents excessive movement in overactive muscles, allowing them to relax. In dentistry, injecting botox type into the chewing muscles effectively reduces involuntary contractions that contribute to jaw pain, bruxism, and TMJ disorders. The brain may still signal muscle movement, but with the release of acetylcholine blocked, the muscles are unable to contract with the same intensity. This results in a significant decrease in strain and tension, alleviating discomfort and improving jaw function. By targeting the root cause of excessive muscle activity, Botox provides a non-invasive solution for managing persistent jaw-related pain and dysfunction.
How Does Botox Treat TMJ?
Botox injection of the masseter muscle to treat muscle pain caused by bruxism.
Botox provides relief for patients suffering from TMJ disorders by targeting the overactive muscles responsible for jaw tension and pain. When injected into specific areas, Botox works by temporarily reducing excessive muscle contractions, preventing the clenching and grinding that often leads to persistent discomfort. Many patients experience symptoms such as jaw tightness, chronic headaches, and excessive tooth wear—issues that stem from the continuous overuse of the masticatory muscles. By relaxing these muscles, Botox alleviates strain on the temporomandibular joint and reduces the pain associated with bruxism and muscle hyperactivity.
During routine dental examinations, dentists can identify potential TMJ issues by assessing signs of excessive wear on the teeth, gum recession, and muscle hypertrophy in the masseter and temporalis muscles. Enlarged chewing muscles, along with tenderness upon palpation, are strong indicators of chronic overuse and potential TMJ dysfunction. Botox injections offer an effective, minimally invasive solution for managing TMJ symptoms, allowing patients to regain comfort and function in their daily lives.
Types of Botox
When Botox first entered the market, it was exclusively produced by Allergan, the company behind the well-known brand. Over time, other manufacturers developed similar formulations of botulinum toxin, creating alternatives that function in much the same way. Today, much like how the word "Kleenex" is used interchangeably for facial tissues, the term "Botox" is often used generically to refer to different brands of botulinum toxin treatments. While Botox with a capital 'B' refers specifically to the Allergan product, lowercase "botox" is commonly used to describe similar products from other companies.
Several botulinum toxin formulations are now widely used by healthcare professionals for dental, medical and cosmetic applications. These include:
Botox (onabotulinumtoxinA) – The original formulation, known for its reliability in reducing muscle contractions.
Dysport (abobotulinumtoxinA) – Diffuses slightly more than Botox, making it a preferred choice for larger treatment areas.
Xeomin (incobotulinumtoxinA) – A purer formulation that lacks accessory proteins, reducing the risk of resistance over time.
Jeuveau (prabotulinumtoxinA-xvfs) – A newer alternative, often marketed as "Newtox," offering similar results to Botox.
Each of these options is used to ease pain and relieve TMD symptoms by relaxing overactive muscles and preventing excessive contractions. The choice of formulation depends on a variety of factors, including the patient's individual response, treatment goals, and the diffusion properties of the product. Dentists incorporating botulinum toxin into their practice should consider these differences to ensure optimal results for their patients.
Will Therapeutic Botox Fix My Wrinkles?
While Botox is primarily known for its therapeutic applications in pain management, it also offers noticeable cosmetic benefits. Patients receiving Botox treatments for TMJ disorder or bruxism often experience a reduction in facial wrinkles due to muscle relaxation. Botox, along with similar formulations like Xeomin, Jeuveau, and Dysport, is FDA-approved for treating both medical conditions and aesthetic concerns. Specifically, it is used to minimize the appearance of crow’s feet around the eyes, frown lines (glabellar lines) between the eyebrows, forehead wrinkles, and vertical platysma bands along the neck.
By blocking nerve signals that trigger excessive muscle contractions, Botox not only helps relieve pain but also softens facial lines that result from repeated movements. This dual effect makes it a valuable option for patients seeking both functional relief and a smoother, more youthful appearance. Although the primary goal of therapeutic Botox is to alleviate discomfort associated with TMJ disorders, its ability to reduce the visibility of wrinkles is a welcomed benefit for many patients. A healthcare professional can assess individual needs and tailor Botox treatments to achieve both therapeutic and aesthetic results.
How Long Does Botox Last?
Botox treatments typically last around three months, after which patients may begin to notice the return of symptoms such as headaches, jaw clenching, and teeth grinding. The duration of effectiveness is a natural function of how Botox interacts with the muscles, gradually wearing off over time. To maintain optimal relief, patients are encouraged to receive Botox injections every three months, especially during the first year of treatment. Over time, as the treated muscles become smaller and less prone to excessive contraction, the frequency of treatments can often be reduced to once or twice per year.
Incorporating complementary therapies, such as physical therapy techniques and targeted muscle stretching, can further enhance the longevity of Botox’s effects. Stretching the masseter, medial pterygoid, and temporalis muscles helps to elongate the fibers, reducing their tendency to contract forcefully. Additionally, using muscle relaxants when necessary can support muscle recovery and relaxation, while addressing secondary symptoms such as neck aches that may accompany chronic jaw tension. Long-term Botox treatment can also contribute to better control of the lower jaw, helping patients experience sustained relief from TMJ-related muscle pain.
How Often Do I Need Botox?
For most patients, Botox treatments are administered every three to four months. However, individual responses vary, and some may require more frequent treatments, especially during the initial phase of therapy. Dentists should assess patient progress and adjust treatment schedules accordingly.
Can Dentists Administer Botox?
Dentists have been using Botox for years to treat muscle-related dental issues, including TMJ disorders and bruxism. While healthcare providers in various fields use Botox for medical conditions such as migraines and excessive sweating, dentists specifically administer it to ease pain and improve TMD pain by relaxing the overactive muscles of mastication. The ability of Botox to reduce excessive muscle contractions makes it an effective treatment for patients suffering from jaw-related discomfort and dysfunction.
Each state has specific regulations regarding the administration of Botox by dentists. In many states, including California, dentists are permitted to use Botox for therapeutic purposes, particularly in treating conditions affecting the muscles of mastication. However, cosmetic applications are often restricted to plastic surgeons and other medical professionals. Many patients who receive Botox injections from neurologists for migraine relief may continue to experience TMJ-related muscle pain because neurologists typically do not target the chewing muscles. Dentists, with their expertise in oral and facial anatomy, are uniquely positioned to address these concerns and provide comprehensive treatment solutions.
To learn more about the dental board position in your state, dentists should consult their state’s dental board website or contact the board directly to review current regulations, scope-of-practice guidelines, and continuing education requirements related to Botox administration for therapeutic use.
How to Learn Botox for Dentists
Finding a course that teaches dentists how to use Botox effectively is the first step in integrating this treatment into a dental practice. While many training programs focus primarily on cosmetic applications, learning how to use Botox for therapeutic purposes—such as treating TMJ disorders, bruxism, and orofacial pain—is essential for dental professionals.
I offer a specialized online course through Dental Practice Mastery that is designed specifically for dentists who want to use Botox as a therapeutic tool. My program focuses on the treatment of facial muscles involved in mastication and jaw function, ensuring that dentists gain a deep understanding of how to administer Botox safely and effectively for pain relief. The course is structured to be accessible at your own pace, allowing you to learn when it’s most convenient for you.
One of the key benefits of my program is the mentorship component. Every month, participants have the opportunity to join live discussions, ask questions, and review case studies directly with me. Additionally, the course includes access to an exclusive online community where you can collaborate with other dental professionals, share insights, and seek guidance as you refine your skills. If you're ready to expand your practice and help patients with a proven, nonsurgical treatment for TMJ disorders, you can learn more about my course at Dental Practice Mastery.
Orofacial Pain Organizations
When it comes to treating TMJ-related muscle pain with Botox, it’s essential for dentists to receive comprehensive, evidence-based training. Understanding the complexity of orofacial pain requires more than a single course—it involves drawing from a range of credible educational sources and tailoring that knowledge to each individual case. A healthcare provider must be able to assess a detailed medical history, monitor when symptoms worsen, and apply safe and effective treatment protocols. My personal journey in mastering the use of Botox for TMJ-related myalgia began with foundational training through respected institutions and continued through my clinical experience and teaching.
Some of the most reputable organizations offering education in orofacial pain and Botox therapy include:
The American Academy of Facial Esthetics (AAFE)
The Aesthetic Learning Center
University of Southern California Herman Ostrow School of Dentistry – Mini Residency in Orofacial Pain
Dental Practice Mastery – Botox for Dentists (Course created by me, combining years of training and practical application)
By studying with these programs, dental professionals—whether early in their careers or alumni of a dental school—can develop the expertise needed to provide effective care for patients suffering from TMJ-related conditions.
What Techniques Are Used When Administering Botox for Therapeutics?
Video Credit: Dental Practice Mastery/Instagram
Administering Botox for therapeutic purposes requires precision and a thorough understanding of facial anatomy. The first step is a comprehensive muscle examination to assess the patient’s pain levels and identify the specific muscles contributing to TMJ-related muscle pain. Healthcare professionals palpate the muscles and ask patients to describe their pain intensity—whether mild, moderate, or severe. If pain is referred to a different location, this indicates the presence of trigger points, which may also benefit from Botox treatment.
Before proceeding with injections, it is crucial to rule out other medical conditions that could be causing facial pain, such as trigeminal neuralgia or chronic migraines. A structured assessment, such as the Visual Analog Scale (VAS), is used to document the patient’s response to a series of anesthetic challenges. The VAS provides an objective method for evaluating pain relief by having patients rate their discomfort on a scale from no pain to intense pain. Initially, the patient records their pain level without any treatment. Then, different anesthetic challenges—such as ethyl chloride spray, muscle stretching, laser treatment, dry needling, and trigger point injections with lidocaine—are administered sequentially. After each intervention, the patient rates their pain again, with previous responses concealed to prevent bias. If these treatments provide temporary relief, it strongly suggests that the affected muscles will respond well to Botox injections for long-term management.
The injection technique involves carefully targeting the affected jaw muscles while avoiding adjacent muscles responsible for essential functions such as smiling and facial expressions. For example, when injecting the masseter muscle, the provider grasps the muscle to locate the most prominent area before administering Botox. Similarly, injections into the temporalis muscle must be placed with precision to ensure effective relief while preserving normal muscle function. Special care is taken to avoid mistakenly injecting muscles such as the risorius, which controls smiling—improper injection could temporarily impair a patient’s ability to smile for several months.
By using a systematic approach that includes muscle examination, VAS-guided anesthetic challenges, and precise injection techniques, dentists can effectively administer Botox to treat severe symptoms of TMJ-related muscle pain, relieve jaw locking, and improve patients' overall comfort and function.
Botox vs. Night Guards To Treat TMJ Pain
For years, the go-to treatment for bruxism and teeth clenching has been the use of oral splints—commonly known as night guards. These devices are designed to act as a protective barrier between the upper and lower teeth, helping to reduce the damage caused by nighttime grinding. However, despite their widespread use, patient compliance with night guards is notoriously low. Many individuals find them uncomfortable, and it’s not uncommon for patients to remove them subconsciously during sleep, only to discover the device on the floor or under the bed by morning. In contrast, Botox offers a more dependable solution. Once injected into the overactive jaw muscles, it works continuously without requiring any effort or cooperation from the patient. Botox automatically reduces muscle activity, making it an ideal option for those struggling with acute pain caused by chronic bruxism. It also bypasses the behavioral triggers like gum chewing and nail biting that can aggravate jaw tension. For patients who are noncompliant with traditional mouth guard use, Botox presents a more consistent and effective approach to managing TMJ-related muscle pain.
Botox for TMJ Injection Sites
Video Credit: Dental Practice Mastery/Instagram
Which Muscles Are Treated?
Masseter Muscle
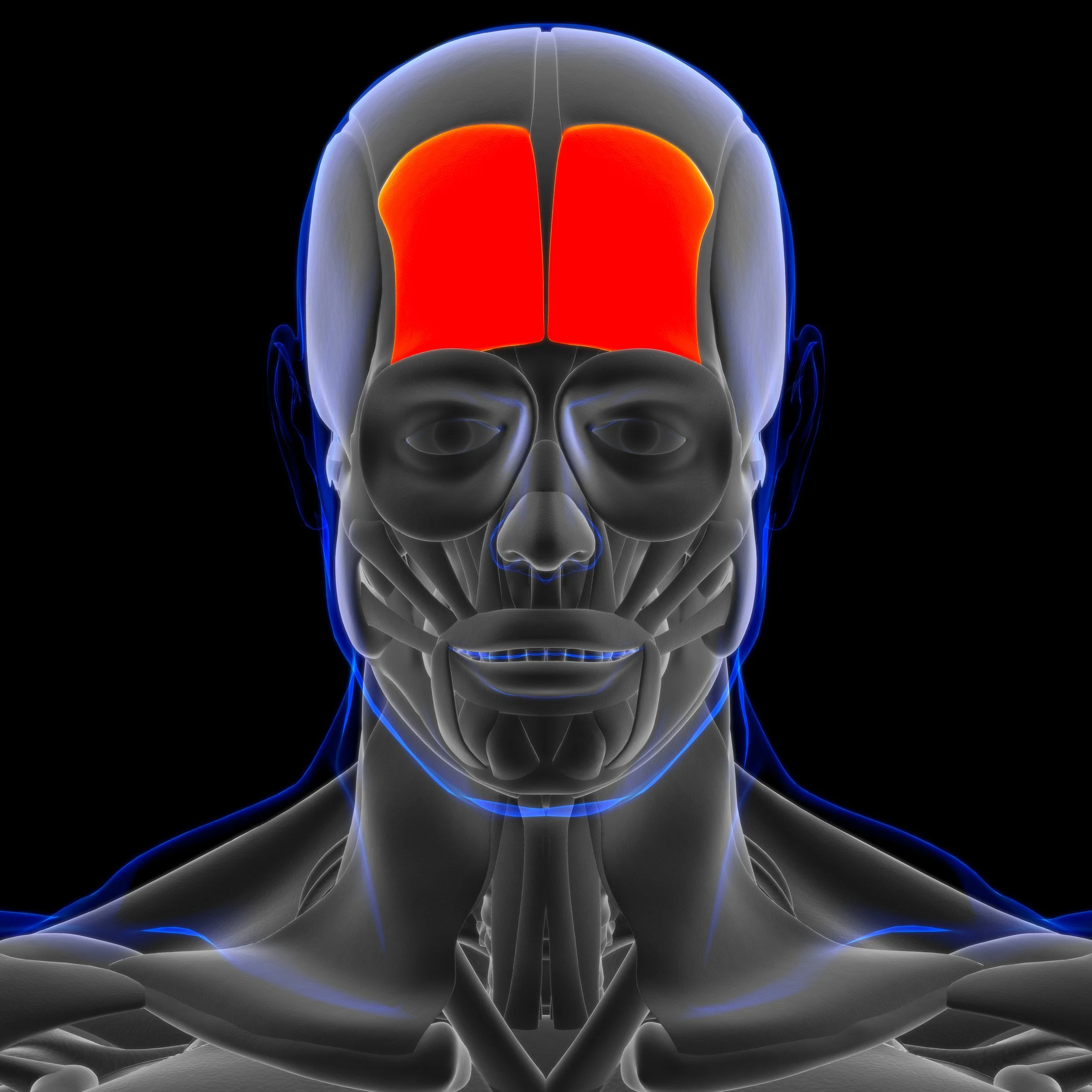
When treating TMJ-related muscle pain with Botox, careful attention is given to the injection sites to ensure maximum effectiveness and patient relief. There are nine key head and neck muscles commonly targeted during treatment, with the primary focus on the muscles of mastication—specifically the masseter, temporalis, and medial pterygoid muscles. These are the main contributors to jaw tension and grinding. While the lateral pterygoid is also a muscle of mastication, its deep anatomical position makes it less commonly injected. In addition to these chewing muscles, several head and neck muscles—such as the splenius capitis, semispinalis capitis, and sternocleidomastoid—are often overworked in patients suffering from bruxism and chronic jaw clenching. These muscles, when strained, can contribute to severe pain and stiffness that radiates through the neck and shoulders.
Facial expression muscles like the orbicularis oculi, corrugator, procerus, and frontalis may also be injected in cases where bruxism affects surrounding soft tissue and contributes to tension headaches or facial discomfort. Botox provides an effective non-invasive option among other procedures, offering targeted muscle relaxation to reduce strain and improve function. By injecting these specific sites, healthcare professionals help patients achieve meaningful pain relief while also complementing other relaxation techniques and long-term TMJ management strategies.
When treating TMJ-related muscle pain with Botox, a thorough muscle examination is conducted to identify the specific muscles contributing to discomfort. There are nine primary muscles that may be evaluated and treated, progressing from the lower regions of the body upward.
Sternocleidomastoid Muscle
The assessment begins with the trapezius muscle, which extends from the neck to the shoulders and plays a role in overall postural stability. Next, the sternocleidomastoid (SCM) muscle, located along the side of the neck, is examined, as it can contribute to jaw tension and headaches. Moving inward, the medial pterygoid and masseter muscles—both critical for chewing—are evaluated. The superficial masseter and deep masseter are further examined, as they are directly involved in jaw clenching and grinding, two common causes of TMJ-related pain.
Trapezius Muscle
The evaluation continues with muscles that impact head and neck function, including the splenius capitis and semispinalis capitis, which are located at the back of the neck and can contribute to referred pain in the jaw. The occipitalis muscle, located at the back of the head at the nuchal line of the skull, is also assessed, as tension in this area can exacerbate TMJ symptoms. Finally, the temporalis muscle, which sits on the side of the head and plays a key role in chewing and jaw movement, is examined.
Medial Pterygoid
Additional muscles of facial expression, such as the corrugator supercilii, procerus, and frontalis muscles, may also be assessed, particularly in patients experiencing associated headaches or facial tension. Since these muscles contribute to TMJ-related pain and overall jaw dysfunction, targeting them with Botox can help alleviate symptoms and prevent the condition from worsening. By carefully identifying and treating the right muscle groups, dentists can provide targeted relief and improve jaw function in patients suffering from TMJ-related muscle pain.
Corrugator Supercilii
Semispinalis Capitis
occipitalis muscle
Temporalis Muscle
Splenius Capitis
Procerus
Frontalis Muscle
Additional Remedies for Treating TMJ-Related Muscle Pain
Video Credit: Dental Practice Mastery/Instagram
While Botox offers long-lasting relief for TMJ-related muscle pain, it may not always be accessible due to cost, especially when repeat treatments are recommended every three months. Fortunately, there are additional remedies that can help manage symptoms and extend the effects of Botox or serve as alternatives when needed. One such approach is incorporating muscle stretching, which functions as a form of physical therapy for the head and neck. When combined with other treatments, stretching can help elongate tight muscles, reducing tension and discomfort over time.
Other treatments include trigger point injections, either dry needling or with lidocaine, which can relieve localized muscle pain. Ethyl chloride spray, a sensory distraction technique, provides almost immediate relief by briefly numbing the area and increasing fresh blood flow once the tissue returns to normal temperature. Heating pads can also help relax tight muscles, while low-level laser therapy has been shown to promote natural healing and reduce inflammation. These therapies are particularly effective when used together—for example, applying ethyl chloride before stretching enables patients to open their mouths wider with less discomfort, making the stretch more effective.
Lifestyle modifications also play an important role in reducing TMJ pain. Patients are advised to eat soft foods to minimize strain on the jaw muscles and avoid habits like chewing gum or wide yawning, which can trigger muscle overuse. While these approaches may not completely replace Botox, they can significantly improve daily comfort and serve as part of a well-rounded treatment plan. In some cases, over-the-counter pain medications may also be used under a healthcare provider’s guidance to manage flare-ups.
Conclusion
Botox has redefined the way dental professionals approach TMJ-related muscle pain, offering a reliable, nonsurgical treatment that targets the root cause—overactive and strained muscles. By addressing the underlying neuromuscular tension within the TMJ structure, Botox reduces involuntary contractions that lead to pain, stiffness, and dysfunction. This guide has explored the clinical benefits, techniques, injection sites, and complementary strategies that make Botox a powerful tool for managing orofacial discomfort.
Dentists who integrate Botox into their practice are equipped to provide more complete care, especially for patients who haven’t responded well to traditional interventions like night guards or oral splints. Whether used alone or in conjunction with stretching, laser therapy, or lifestyle changes, Botox offers a path to greater comfort, improved jaw function, and better quality of life. With proper training and continued education, dental professionals can confidently utilize Botox to expand their therapeutic capabilities and support patients in achieving lasting relief.